Torticollis
Torticollis is a condition most commonly diagnosed in infancy in which the baby’s head is consistently tilted or turned to one direction. It is often present beginning at birth, but is typically noticed at 1-2 months of age as the baby’s head control improves. The most common cause is tightness in the neck muscles due to a variety of potential factors.
Torticollis risk factors:
- Positioning in utero
- Delivery in breech position or use of forceps for delivery
- Multiples birth (twins, triplets, etc.)
- Reflux (GERD)
- Vision concerns
- Genetic factors and syndromes
Signs of torticollis:
- Baby or child consistently tilts head towards one side in most positions
- Baby or child consistently turns head (rotates) or looks in one direction
- Baby has difficulty bottle feeding or breastfeeding on one side noted
- Baby has a flat spot on the head
- Baby has asymmetries in the head and facial region
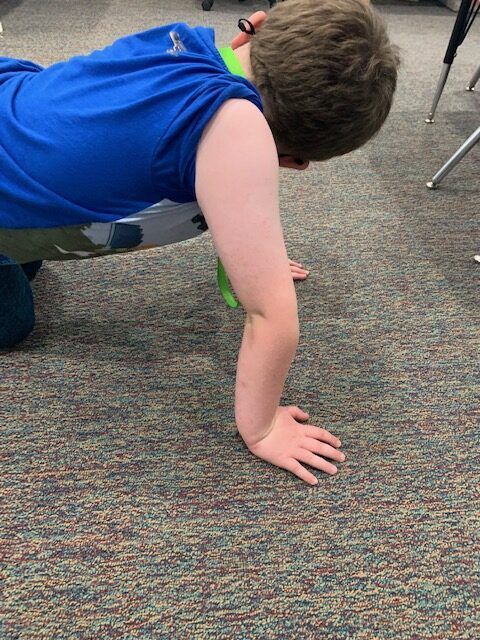
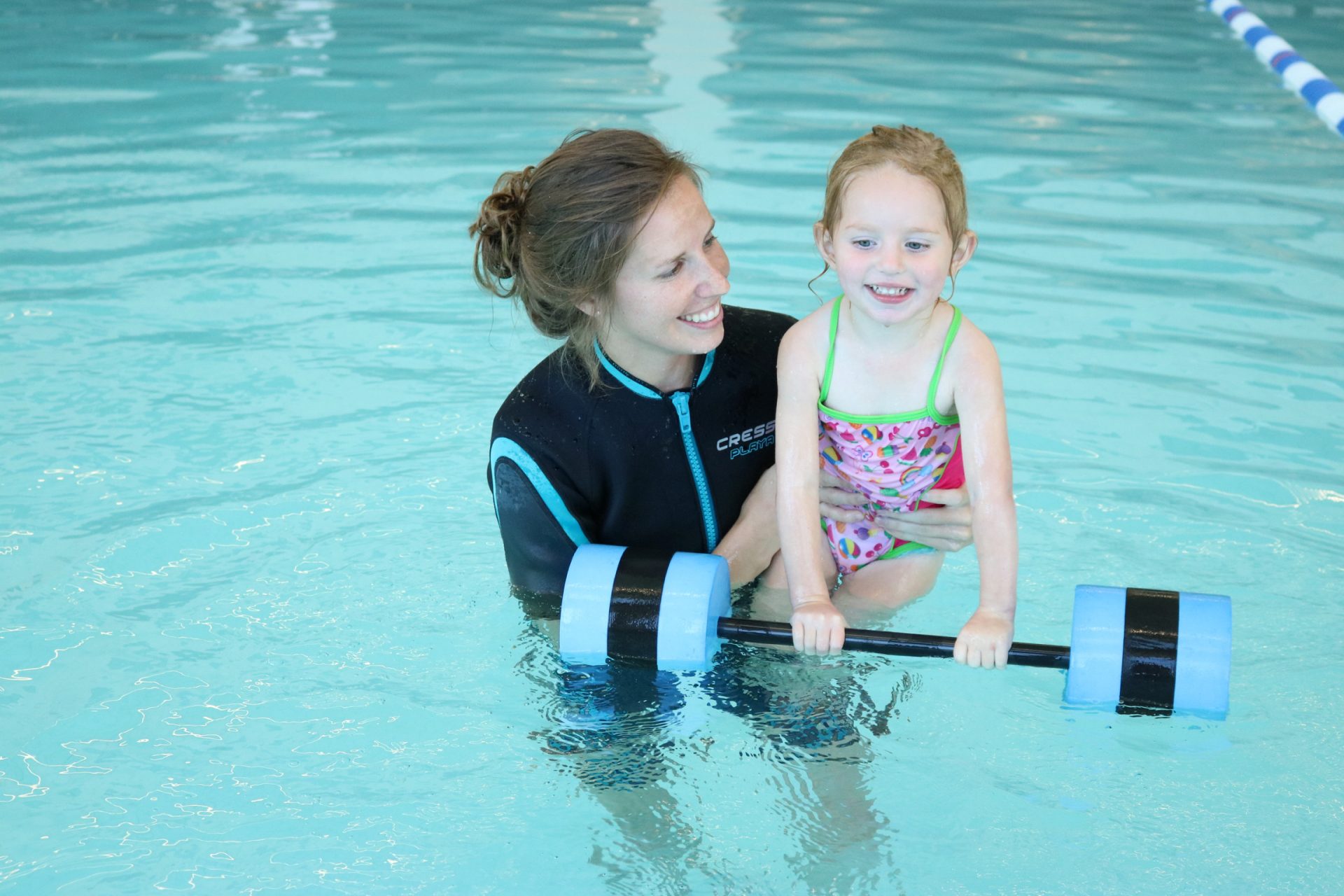
Torticollis can be treated by a pediatric physical therapist (PT). Your PT will work with you and your baby to create an individualized plan of care including stretching and strengthening activities for your baby’s neck and trunk. Improvements in strength and head position are typically noted within the first few months of physical therapy with a good prognosis to completely resolve the torticollis, especially if treated early. If left untreated, torticollis can impact the following areas of development: rolling, sitting, pulling to stand, crawling, standing, walking, balance, vision, bottle feeding and breastfeeding, and eating.
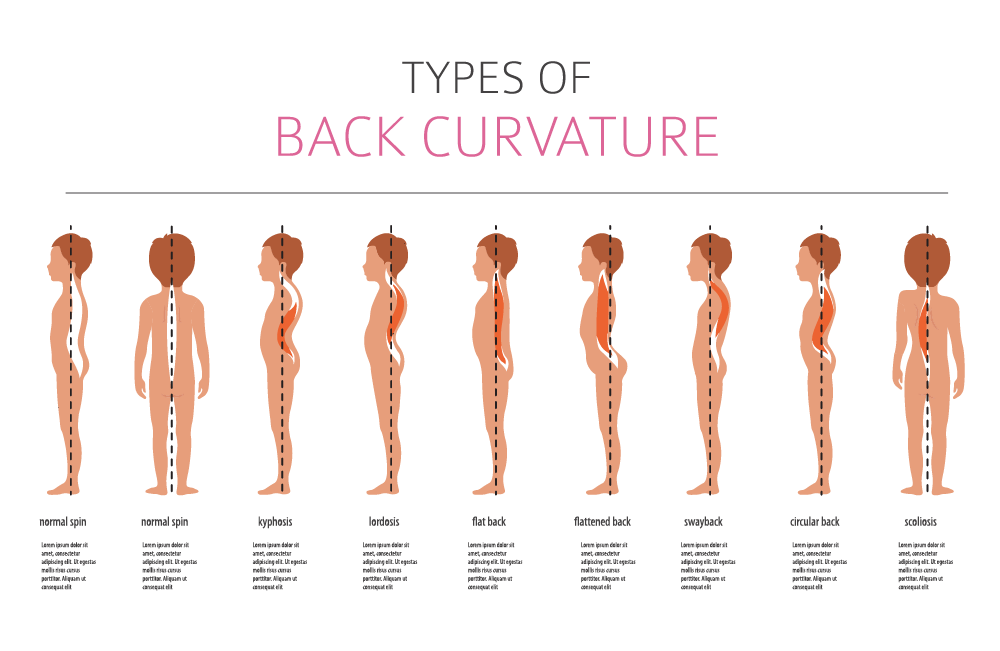
Conditions associated with torticollis:
It is never too early to intervene and to treat torticollis. Schedule a free screening with a physical therapist at BDI Playhouse if you have any questions about your baby’s head position or head shape. So worry not, our BDI Playhouse therapists are experts in this area and we are waiting to answer any questions you may have!
Written by: Cassidy Bannon, PT, DPT