Incontinence
Pediatric Incontinence
& Pelvic Floor Health:
Accidents, Bedwetting, and Constipation
Does your child struggle with bedwetting, accidents, and/or constipation?
Pelvic floor physical therapy might be your answer
Pelvic floor physical therapy might be your answer
What is pelvic floor physical therapy for kids?
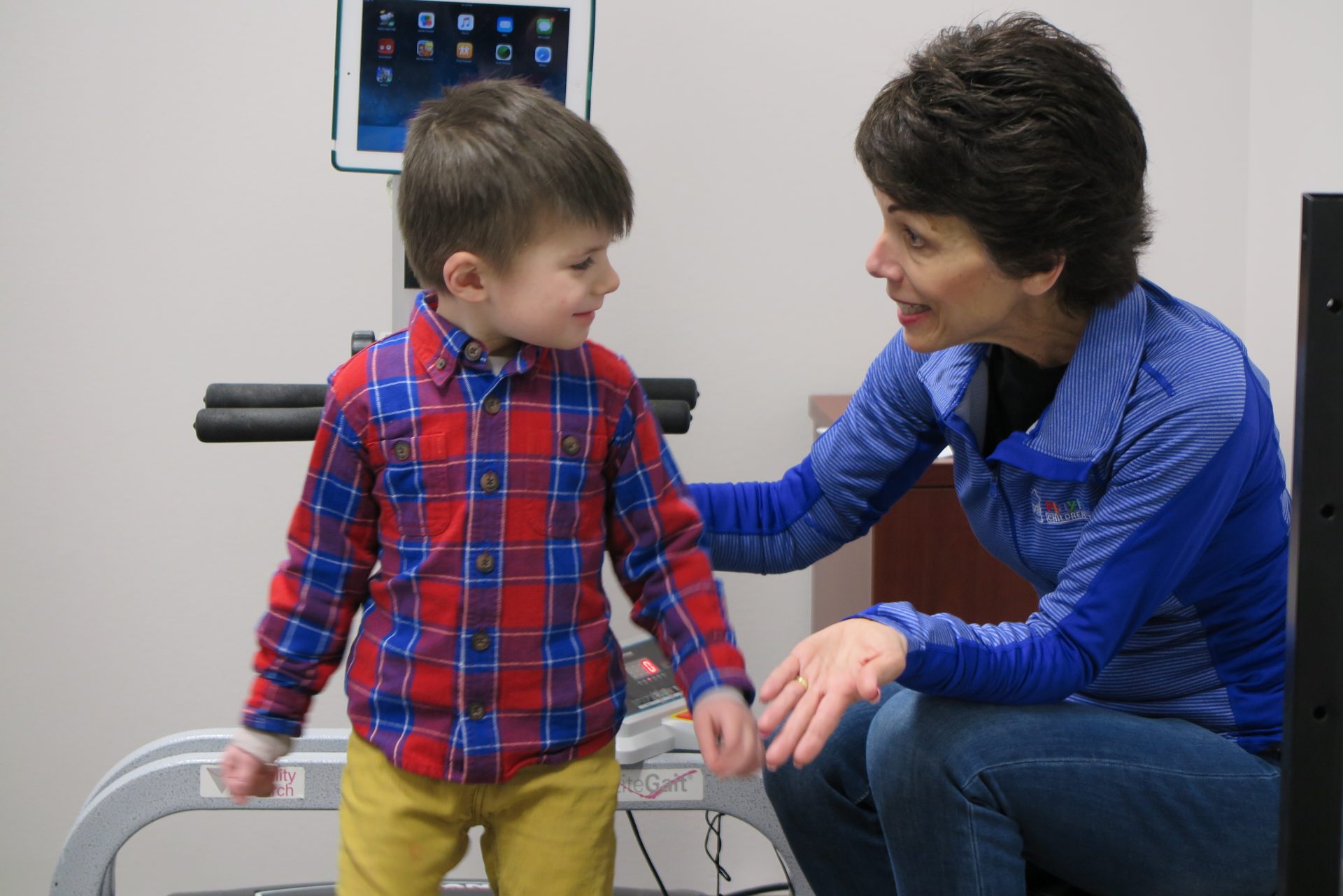
Pediatric pelvic floor physical therapy is a specialized form of physical therapy that focuses on the pelvic floor muscles in children. These muscles help with bowel and bladder control during the day and night.
What makes pediatric pelvic floor therapy different from adult pelvic floor therapy?
The biggest difference in adult and pediatric pelvic floor therapy is that sessions for children include external examinations only. This means that examinations and treatment can be done with out removing the child’s clothing. We make sure to avoid making the child uncomfortable or embarrassed. Sessions focus on education and exercises in a motivating environment. Parents are welcome to be present during all evaluations and sessions.
Why would my child need to see a pelvic floor therapist?
- Bedwetting after age 5
- Bowel or urinary accidents (incontinence) during the day after being potty trained
- Constipation
- Decreased awareness of bowel or bladder urge
- Not being able to hold urine after sudden urge
- Urinary leakage with exertion such as jumping
What happens during an evaluation?
Interview with the child and caregiver
An interview with the child and caregiver is completed at the beginning to review the child’s medical history, symptoms, and any previous treatments. Goals are discussed and based on each family’s concerns.
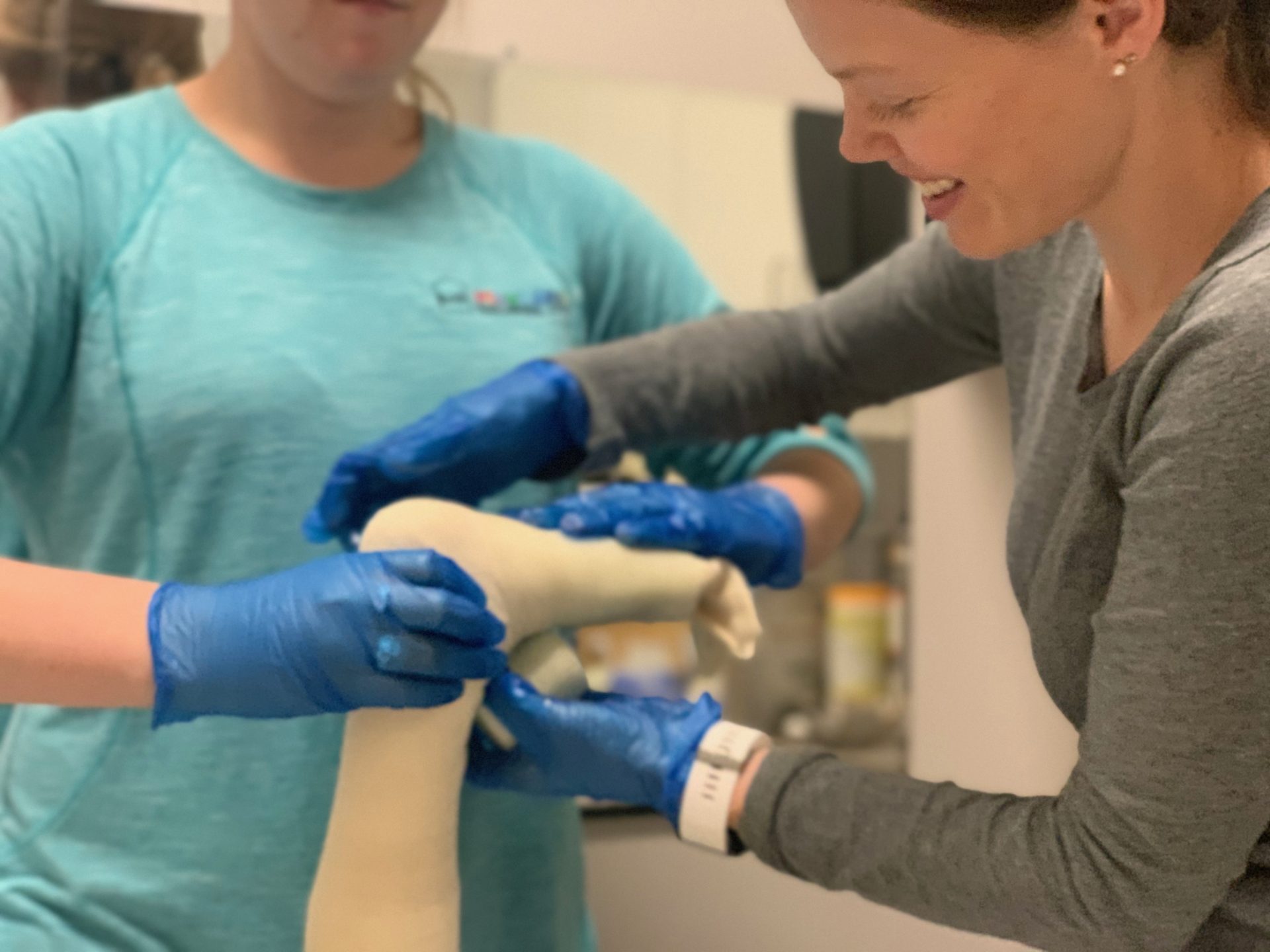
Physical examination
Following the interview, a physical examination is performed to evaluate the child’s movement and overall functioning. This typically includes observing posture and movement patterns, as well as assessing muscle strength and flexibility. The therapist also checks for any signs of pain or discomfort in the pelvic region. Throughout the evaluation, children remain fully clothed and are encouraged to demonstrate seated posture using various clinic equipment. Sessions can take place in a private room or a shared gym space, depending on the child’s comfort and preference.
How do therapists address accidents, bedwetting, and constipation with pelvic floor therapy for kids?
Our therapists incorporate a holistic approach that includes diet, posture retraining, sleep patterns, and other behavioral conditions that could be impacting the child’s continence. Our multidisciplinary team is able to collaborate to determine the best strategies for each child. These strategies may include:
Core strengthening
Biofeedback
Bladder re-training
Behavior and diet strategies
Body awareness to help realize the urge to go
Posture training
Sensory strategies to assist with tolerance for public bathrooms and toileting
Review of bathroom setup
Bowel and bladder logs
Increasing variety of foods and limiting bladder irritants
Modified O’Regan Protocol assistance
What is biofeedback?
Biofeedback can be used to help children learn to relax and contract their muscles effectively in order help them use the bathroom more efficiently. Little stickers, electrodes, are attached to their muscles and give feedback to a computer. This feedback is connected to a game that responds to the child’s relaxation or contraction of specific muscles. Biofeedback is commonly used for pediatric incontinence, but can also be used for body awareness to help strengthen specific muscles. Biofeedback sessions occur in a private treatment room with an adult caregiver present. Electrode placement is external and only completed with child and caregiver consent.
Modified O’Regan Protocol (M.O.P.)
We have a M.O.P. ( Modified O’Regan Protocol) specialist, Andrea Turnell, PT, DPT, on staff that can support your child’s M.O.P journey and assist in interpreting your process!
Questions about Pelvic Floor Therapy?
[receiver]