Primitive Reflexes
Primative Reflexes- The Good, The Bad, The Better!
Have you ever tripped and simultaneously reached out your hands to stop the fall? That is your primitive reflexes at work! They are essential as the first line of defense to protect ourselves but they can also be detrimental to our development.
What are primitive reflexes?
Primitive reflexes are involuntary motor responses present at infancy that facilitate survival. Pediatricians check these reflexes at wellness visits to ensure the nervous system is working properly. It is important that these reflexes are present but it is just as important that these reflexes mature or integrate in early childhood.
The Good:
REFLEX | GOOD |
| Moro Reflex The startle reflex | A fear response to sudden movements or noise |
| Hands Pulling | Head control reflex and the ability to contract our muscles to sit up |
| Hands Supporting | Our falling reflex. Ability to reach out and catch yourself. |
| Tonic Labyrinthine (TLR) | Develops balance and spatial awareness |
| STNR | Head, limbs and balance system connection |
| Asymmetrical Tonic Neck Reflex (ATNR): | Differentiates our left and right side. |
| Spinal Galant | Connects the trunk and lower body |
| Amphibian | Activates nerves between both hemispheres of the brain |
| Babinski: | Supports mature walking and balance |
| Babkin | Tongue and mouth coordination for eating and speaking |
| Plantar | Protective response to provide stability |
| Palmar | Advances fine motor movements of fingers. |
| Landau | Promotes ability to control head in tummy time |
Why do reflexes need to integrate?
We unconsciously use these reflexes everyday, but what happens when we are unable to consciously control them? That’s what happens when reflexes don’t integrate. It’s like being in a self driving car and not being able to take control of the wheel, which can be very scary. Sometimes our reflexes do not mature because of abnormal movement patterns in utero or infancy, neurological deficits, or just unknown reasons. These primitive neuro connections are powerful and can inhibit our ability to voluntarily control our body and mind if they are retained.
How do reflexes affect development?
A retained reflex can present in strange ways causing possible behavioral, emotional, sensory and physical deficts. Not all reflexes present the same way in every person but they do have common patterns. The infant’s movements work together in sequence during development. If one reflex does not integrate it can cause others to also be retained. It is not uncommon to see two, three, or almost all the reflexes present during a primitive reflex evaluation. The following are common traits you might see if reflexes are retained.
The Bad- Unintegrated Primative Reflexes
REFLEX | GOOD | BAD |
| Moro Reflex The startle reflex | A fear response to sudden movements or noise |
|
| Hands Pulling | Head control reflex and the ability to contract our muscles to sit up |
|
| Hands Supporting | Our falling reflex. Ability to reach out and catch yourself. |
|
| Tonic Labyrinthine (TLR) | Develops balance and spatial awareness |
|
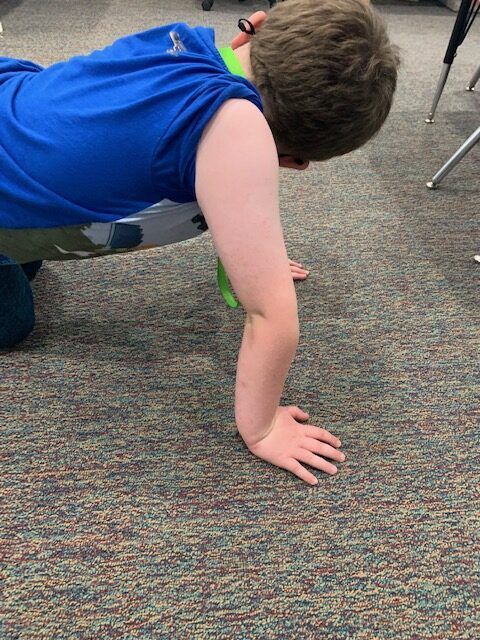
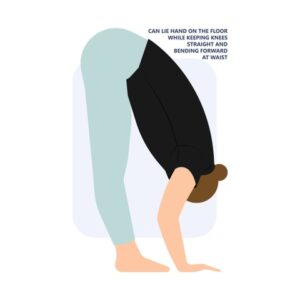
| STNR | Head, limbs and balance system connection |
|
| Asymmetrical Tonic Neck Reflex (ATNR): | Differentiates our left and right side. |
|
| Spinal Galant | Connects the trunk and lower body |
|
| Amphibian | Activates nerves between both hemispheres of the brain |
|
| Babinski: | Supports mature walking and balance |
|
| Babkin | Tongue and mouth coordination for eating and speaking |
|
| Plantar | Protective response to provide stability |
|
| Palmar | Advances fine motor movements of fingers. | |
| Landau | Promotes ability to control head in tummy time |
|
The Better:
It is extremely common to have one or more reflexes present and you might even identify some of these traits in yourself. That does not mean it needs to be treated unless the reflex is so dominant that it interferes with the ability to learn, be safe and thrive. Reflex therapy helps to identify and create an individualized reflex exercise program to promote integration. The brain responds by taking the wheel and improves control over it’s own mind and body. Now that’s better!
If you think your child may have primitive reflexes present we can help! Free primitive reflex screenings are available via Zoom or in person at our Orland Park or Naperville/Aurora locations.