When to see a pediatric physical therapist for your child’s feet?
How do you know if your child’s little feet are functioning at their very best? Here are 10 clear signs that you should have a pediatric physical therapist screen your child’s feet so they can put their best foot forward!
Pain
If walking causes pain in your child’s feet this is a concern that should be addressed immediately. There are a number of reasons for pain in the feet and a pediatric PT can assess and address painful walking.
Asymmetry
Any difference in one foot compared to the other foot should be seen by a pediatric PT. Feet should look and move the same at the other foot. Seek advice if you notice a difference in foot size, a heel lifted on one side, turning in or out of one foot or any other noticeable differences.
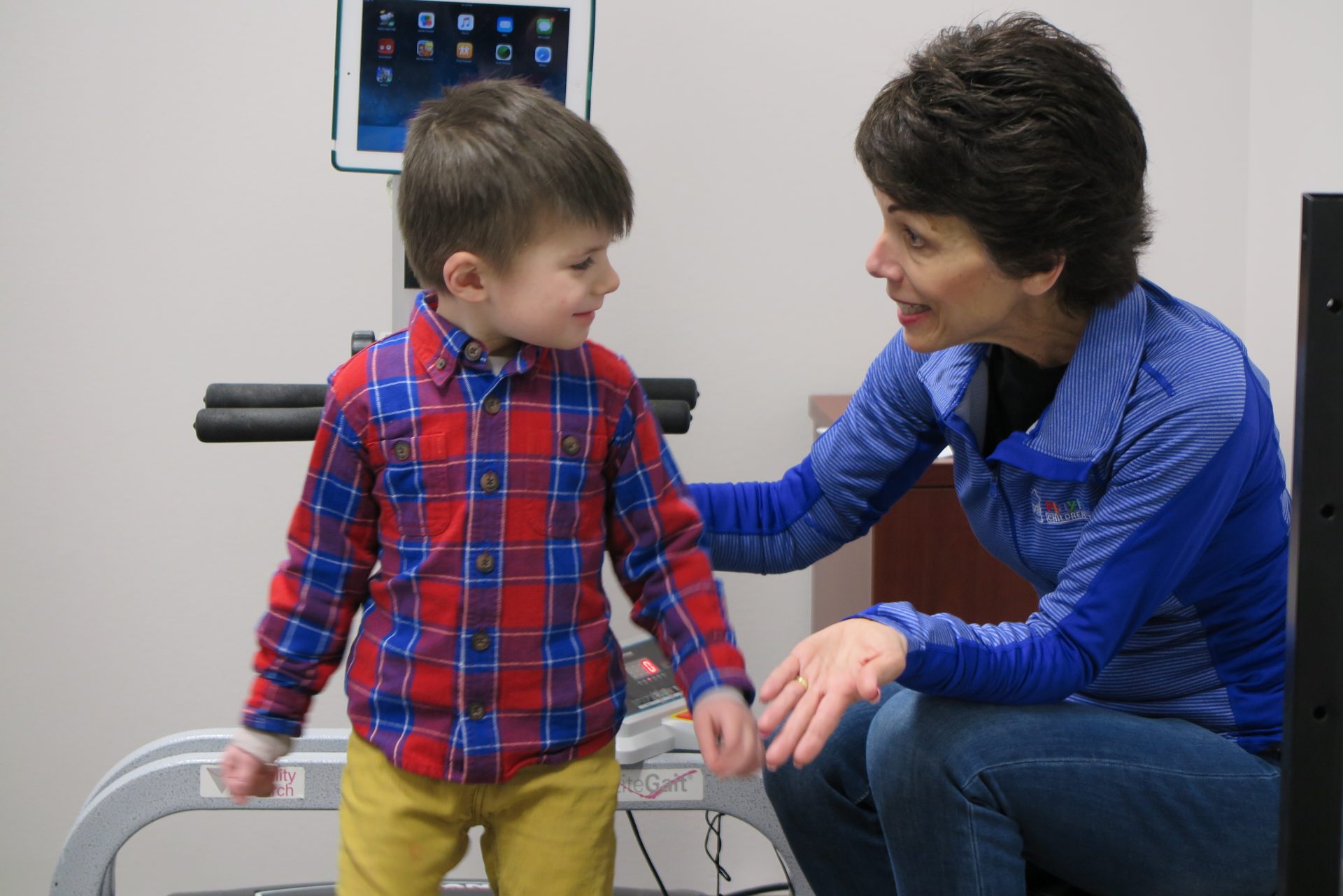
Toe Walking
Toe walking is an abnormal gait or walk at any age at any time! We often see children raise up on their toes when they are very excited, nervous or cold but only for a few steps and then come down to their heels to walk or run. The earlier a child is seen for toe walking, the faster the treatment and the better the outcome. Don’t Wait!
In or Out Toeing (Pigeon or Duck footed)
Toe inning or outing is a common foot alignment deficit. When the feet are not aligned, the knees are not aligned which can lead to pain and inflammation. Often it can be a sign of leg, hip or trunk weakness or all three! It could also be a misalignment of bones within the joints. Seeing a pediatric PTl will determine the root cause and help get those duck feet in a row!
Flat Feet / Pronation
Flat feet is when almost the whole foot makes contact with the floor while standing. Pronation is when the ankle collapses inward when standing. Both flat feet and pronation can cause similar problems. Postural deficits are usually present as well as over use and under used muscle groups. This imbalance causes poor body mechanics which can lead to premature breakdown of joints. Flat feet and pronation cause the body to move inefficiently. It will take more energy to walk, run and jump!
Tripping
Children are still developing their sensory systems and body awareness which can look a bit messy. It’s common to miss a crack in the sidewalk or move too fast for their feet causing them to trip and fall. Tripping becomes a problem when they are doing it so much they are hurting themselves. Tripping on the same thing over and over, on stairs or ramps, carpets or even nothing at all can be concerning. A pediatric PT will be able to assess why they are tripping so often and help keep them on their feet!
Fatigues Quickly with Walking
Carry me! Is a phrase often used by a child who fatigues quickly when walking. A child who has good endurance, body mechanics, postural control and strength will want to walk vs being pushed in a stroller or carried. A child who struggles with one or more of these deficits will fatigue quickly when walking and ask to be carried more often. Ask a professional if your child seems to fatigue quickly when walking vs other children their age.
Aversion to changing shoes
New shoes or any new clothing item can be stressful to a developing sensory system. Our children who are more sensitive to change will often break down their favorite pair of shoes to a thin sole, or wear shoes that lack proper support such as slip-on type shoes. A professional can help get children into good quality shoes that support the foot properly, helping them to move with better posture and efficiency. Let’s make shopping for new shoes fun!
Sprained or twisted ankles
This painful injury literally stops you in your tracks. It’s common once in a while but abnormal if it happens over and over again, especially when doing everyday activities. Ankle weakness, misalignment or even vision could be the cause of ankle sprains. A PT can assess and address the reason for this very painful problem.
Abnormal gait / walk
Any abnormality of a child’s gait should be addressed as soon as possible. Sometimes it’s hard to put your finger on it because the smallest thing could be affecting their gait or it comes and goes. Listen for your child’s steps on a hard surface. It should be an even beat most of the time. Rubbing the top of their foot while walking can be a sensory movement that is affecting their gait. Running instead of walking. Gait abnormalities can easily be addressed in PT.
High Arches
High arches do not always need to be addressed but if your child has any other deficits such as any problems above, then high arches may need extra support. A PT can assess their gait and determine if treatment is necessary.
Pediatric Physical Therapists assess the cause of these symptoms and use conservative interventions to improve their everyday function on their feet! They will also refer you to the appropriate healthcare professionals when extra attention is required for the best care of those little feet!
Set up a free screening with a pediatric PT to ensure your child is putting their best foot forward!
Written By: Dana Bukala, PTA